Bone Infection
What is bone infection?
Infection is an invasion of the body by organisms that can cause disease. When bacteria invade a bone, it results in bone infection, also called osteomyelitis. The bacteria eat away at the bone and damage the local blood supply to that bone, which consequently prevents antibiotics from reaching the bacteria to neutralize it.
What causes bone infection?
Bone infection is most often caused by Staphylococcus bacteria. These are commonly referred to as Staph infections. Another name you may have heard is MRSA, which stands for methicillin-resistant Staphylococcus aureus infection. MRSA is caused by a particular bacteria that is resistant to many antibiotics. Bone infection occurs when the bacteria invade bone either through the bloodstream, from nearby infected tissue, or by contact with the outside environment—usually from an open fracture or surgery. While bone infections can also be caused by fungi, it is far less common.
How is bone infection diagnosed?
Bone infection can be difficult to diagnose. Doctors start with a physical exam and then may use blood tests, X-rays, CT scans, and MRIs. Tissue cultures and bone biopsies are helpful to identify the type of bacteria infecting the bone so the doctor can choose the most effective antibiotic to combat it.
How common is bone infection?
Two out of every 10,000 people get bone infections. People with diabetes, rheumatoid arthritis, sickle cell anemia, AIDS and HIV are at increased risk for infection. People with organ transplants who are receiving medication to suppress the immune system and those with multiple medical problems, such as renal and vascular diseases, are also more susceptible. Intravenous drug use is also a risk factor.
What are the symptoms of bone infection?
Bone infection often causes redness, swelling and pain in the affected limb. It can also cause a fever, sweating or chills. Sometimes, fluid exits through the skin; this is called a draining sinus tract. Occasionally the infection weakens the bone so much that the bone breaks.
What are the different types of bone infection?
Infection has several stages, from mild to severe.
- Mild infection does not weaken the structural integrity of the bone and allows safe use of the bone for weight bearing.
- Severe infection eats away at the structural integrity of the bone. When the bone loses its structural integrity, it cannot support weight and will likely break. This can be extremely painful.
Can people live with bone infection? Does it need to be treated?
Bone infection should be treated to try to save the limb and avoid the following possible complications:
- Systemic infection: People can live with bone infection for years as long as the bacteria do not enter the bloodstream and cause the rest of the body to become sick. Signs of systemic infection include fever, chills, rapid heartbeat, and low blood pressure. Systemic spread of bone infection occurs infrequently; it can, however, occur more commonly in a person who becomes weakened from other medical illnesses.
- Infection of other parts of the body: Bacteria that enter the bloodstream can travel to other parts of the body, such as the heart and the joints. The affected heart can become weakened because of damaged valves. The affected joints can become swollen and painful. The bacteria and the white blood cells that fight the bacteria can eat away at joint cartilage if not immediately treated by surgical washing. If the bacteria continue to live in the joints, it is likely that severe permanent arthritis will occur as residual damage.
- Cancer: Infrequently, when bone infection has been present and draining through a sinus tract for years, the skin cells can become cancerous. This type of skin cancer is called a Marjolin ulcer. A bone infection specialist should send surgical samples to the pathology laboratory for evaluation of the potentially cancerous site.
- Osteonecrosis: Literally meaning “bone death,” infection can reduce or stop blood flow to the bone and cause it to die, break down and collapse.
- Septic arthritis (when the bone infection spreads to a joint) and septicemia (blood poisoning).
Is bone infection difficult to treat?
Bone infection can be difficult to treat because bacteria are constantly changing to fight the new antibiotics that are used to kill them. Some bacteria have been extremely difficult to kill, including methicillin-resistant Staphylococcus aureus species and vancomycin-resistant enterococci. These bacteria and their constantly changing genetic makeup make it very difficult to find new antibiotics that will completely eradicate the entire bacterial population.
The primary limitations for success with bone infection treatment are the immune fighting ability of the patient and the circulation of their limbs. Some patients are immunocompromised due to disease (e.g., diabetes, HIV/AIDS) or drugs. Patients who have had organ transplants and are receiving anti-rejection medications, patients receiving steroids for the treatment of other diseases, and smokers are also immunocompromised. Smoking has many negative effects on bone, and delays bone healing; smokers must quit smoking to help ensure a successful result. For more information, see Encouraging Bone Healing.
Can bone infection reoccur?
Even years after successful bone infection treatment, a small area of bone infection can recur, especially if the immune system becomes compromised through illness or poor nutrition.
How is bone infection treated?
The first step to treating an orthopedic infection is to evaluate, and if necessary, optimize the patient’s immune system. If a patient is diagnosed with immune system deficiencies, the patient is referred to an immunologist for treatment to try to boost the immune system. The patient’s nutritional intake should also be supplemented with vitamins and protein to help maximize immunity.
Mild Bone Infection Treatment Steps
- I. Surgical procedure:
- A) Mild infection can be treated with debridement, a surgical procedure that removes all of the infected bone and tissue.
- B) Locally administered antibiotics: Because the bone infection damages the blood supply to the area, oral and IV antibiotics often can’t reach the infected area. Therefore, after the bone is surgically cleaned out, the remaining bone defect is treated with a large dose of antibiotics applied directly to the site of the infection. There are several different ways to apply antibiotics to the area. The antibiotics can be delivered by using non-absorbable bone cement that has antibiotics in it, non-absorbable antibiotic beads, or rods or plates that are coated in antibiotics.
- When these are used, a second surgery will be required to remove them after the bone has healed. Non-absorbable bone cement will also need to be replaced with bone graft by subsequent surgical procedures. An absorbable mix of synthetic bone substitute with antibiotics in it or absorbable antibiotic beads can also be used. These do not need to be later removed by surgery as they will break down over time and help the bone grow after the infection is gone. The doctor will discuss the treatment options and help you select the method that will be most effective for your specific situation.
- II. Oral or IV antibiotic therapy:
- After the bone has been cleaned out and antibiotics have been administered locally, oral or IV antibiotic therapy is required for six weeks to eradicate any remaining bacterial cells in the bone and bloodstream. Once the bacteria that infected the bone has been identified by laboratory results of surgical samples, the doctor will be able to determine which method is necessary.
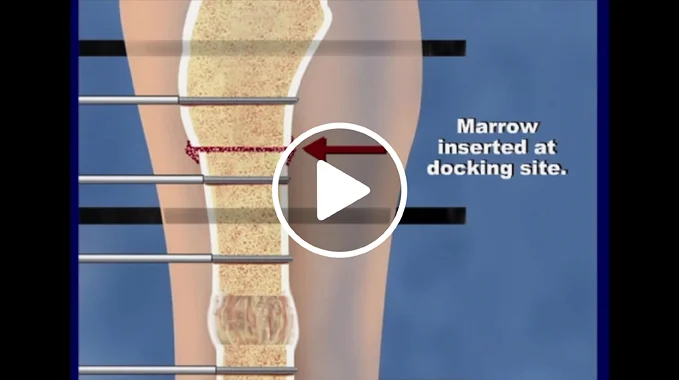
Severe Bone Infection Treatment Steps
- Severe bone infections are also treated with the first two surgical steps of mild bone infections: cleansing out the infected or dead bone and tissue (debridement), and applying antibiotics directly to the infection site. With severe infection, however, the bone is not strong enough to bear weight after debridement.
Many techniques are available to rebuild bone after the bone cleaning procedure has been performed and after antibiotics have been administered locally. Temporary structural stability can be achieved with an external fixator while the infection is being eradicated. Bone rebuilding techniques may also involve bone grafting or bone transport that is achieved with the use of a special Ilizarov external fixator. The fixator can remain in place for several months depending on how much bone was lost from the infection. Just like mild bone infections, severe infections also require six weeks of oral or IV antibiotic therapy that is specific to the bacteria that were present in the bone.
This video helps demonstrate the treatment process:
For more information, please see the Devices & Procedures to Fight Bone Infection section of our website.
Why choose the International Center for Limb Lengthening for treatment of bone infection?
The International Center for Limb Lengthening is a leader in healing patients with bone and joint infections. Dr. Janet Conway is an internationally-recognized expert specializing in the treatment of bone and joint infections and has saved lives and limbs of patients who have failed to heal elsewhere. She has authored and published many papers on the subject and has pioneered numerous innovative treatments for bone infection, including antibiotic-coated rods.
Bone infection treatment can be complex. Your doctor at the International Center for Limb Lengthening will take the time to make sure you understand all your options and then will customize your treatment to meet your specific needs. Our patients benefit from our team-centered approach with world-renowned surgeons and specialized physician assistants, nurses and physical therapists. We help patients with bone infection achieve their best possible result.
Doctors who treat bone infection
†Children and Adolescents/Young Adults Only