Charcot-Marie-Tooth Disease
What is Charcot-Marie-Tooth disease?
Charcot-Marie-Tooth disease is also known as hereditary motor and sensory neuropathy or peroneal muscular atrophy. It is named after the three doctors, Jean Martin Charcot, Pierre Marie and Howard Henry Tooth, who first described this disease in 1886. It is a group of disorders that cause nerve damage to the peripheral nerves in the body. Peripheral nerves carry information between the brain and the muscles. Damaged peripheral nerves result in weakness and deformity of the legs, feet, arms and hands. People with Charcot-Marie-Tooth disease may develop significant difficulty walking.
The disease process involves nerves that are made up of motor neurons that control how our muscles move and sensory neurons that help us sense pressure and pain. Neurons use electrical impulses and chemicals to transmit information through the nervous system. Each neuron has a long, wire-like structure, called an axon that transmits signals. The axon is coated with a protective material called myelin that prevents the electrical signal from losing its strength during transmission. In patients with Charcot-Marie-Tooth disease, the myelin starts to disappear from the axon. This results in decreased signal speed and intensity, leading to muscle weakness, muscle atrophy, decreased sensation and decreased reflexes. The arm and the legs are most affected by this disease.
What are the symptoms of Charcot-Marie-Tooth disease?
Symptoms of Charcot-Marie-Tooth disease usually appear between adolescence and early adulthood. The first symptoms may be of a loss of feeling or muscle weakness in the legs, feet and hands. As weakness progresses, people with the disease may also observe a change in the shape of their feet; many develop a high arch, hammertoes or turning-in of the feet. When left untreated, this may lead to problems with balance, walking and running. Later, the patient may develop a drop foot, rolling of the ankles, and even greater deformity which makes walking very difficult.
Similar symptoms can be found in the hands, which often develop a “crumpled,” flexed look. If Charcot-Marie-Tooth disease affects the patient’s arms and hands, they may develop functional challenges in getting dressed, typing on a computer, turning a doorknob or holding utensils. Usually, patients with the earlier onset of the disease develop the most severe symptoms.
What causes Charcot-Marie-Tooth disease and how common is it?
Charcot-Marie-Tooth disease is usually caused by defects in the genetic materials a person inherits from a parent. However, in some cases, Charcot-Marie-Tooth disease is the result of a non-inherited, spontaneous gene mutation. Either way, Charcot-Marie Tooth disease can be passed on to the next generation. Charcot-Marie Tooth disease is one of the most common inherited neuromuscular disorders, affecting approximately 1 in every 2500 people. There are many variations of the disease.
How is Charcot-Marie-Tooth disease diagnosed?
In order to diagnose Charcot-Marie-Tooth disease, a visit with a skilled clinician is advised. The patient’s health, symptoms and family history are discussed. The patient’s muscular function and gait is evaluated. Follow-up tests should include X-rays to determine if the patient has developed any bone fractures, bone deformities, scoliosis or hip dysplasia. A complete neurological work-up, including nerve conduction studies, electromyography studies and sometimes a nerve biopsy, is also recommended. Genetic testing (“chromosome analysis”) can diagnosis most types of Charcot-Marie-Tooth disease.
What are the treatment options for Charcot-Marie-Tooth disease?
Our goal at the International Center for Limb Lengthening is to help restore as much function as possible to those affected by Charcot-Marie-Tooth disease. Treatment is variable and depends on the specific needs of each individual. Physical therapy, assistive devices and surgical treatment can help people with the challenges they face living with the disease.
Patients most commonly seek medical treatment for foot and gait problems. The first and most common surgical treatment of the feet involves soft-tissue surgery. Soft-tissue surgery corrects the patient’s balance through tendon transfers, muscle lengthening and fascia release. By surgically repairing the muscle imbalances, the patient can return to more functional walking mechanics and motion.
In long-standing, untreated patients, soft-tissue imbalance can lead to bony deformities. In this type of situation, surgery is needed to achieve normal balance. This can be done through osteotomies (bone cuts), bone fusion and with controlled realignment of the bones. Later in life, arthritic joints may become an issue in the feet, and ankle joint replacement becomes a therapeutic possibility.
Why choose the International Center for Limb Lengthening for Charcot-Marie-Tooth disease treatment?
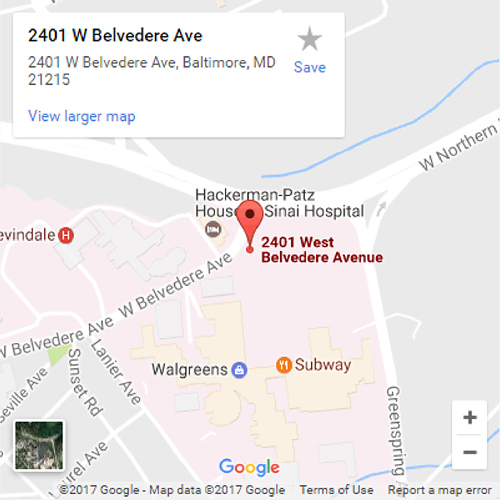
With a collective experience of over thirty years of helping patients with complex lower leg, foot and ankle problems, the Foot and Ankle Service of the Rubin Institute is one of the leading treatment centers for foot and ankle conditions in the United States. Your doctor will take the time to make sure you understand all your options and then will customize your treatment to meet your specific needs. Our patients benefit from our team-centered approach with world-renowned surgeons and specialized physician assistants, nurses and physical therapists. We help patients with Charcot-Marie-Tooth disease achieve their best possible result.
Doctors who treat Charcot-Marie-Tooth disease
‡Adults Only
*Patients Over 16 Years Old Only
†Children and Adolescents/Young Adults Only