External Fixators
What are external fixators?
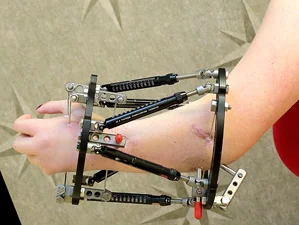
External fixators are metal devices that are attached to the bones of the arm, leg or foot with threaded pins or wires. These threaded pins or wires pass through the skin and muscles and are inserted into the bone. The majority of the device is outside of the body, which is why it is called an external fixator. Many people only require one external fixator to be applied, but some will need two or more external fixators.
When are external fixators used?
External fixators can be used to gradually lengthen a bone, straighten a deformed bone or reduce pressure on a joint through joint distraction.
How are external fixators applied?
During surgery, the doctor will make small incisions and then insert pins or wires into the bone. The external fixator frame will be attached to these pins and wires and secured using clamps and rods. If the bone is to be lengthened or straightened, the doctor will then surgically cut the bone (osteotomy) to create two separate bone segments.
What happens after the external fixator is applied?
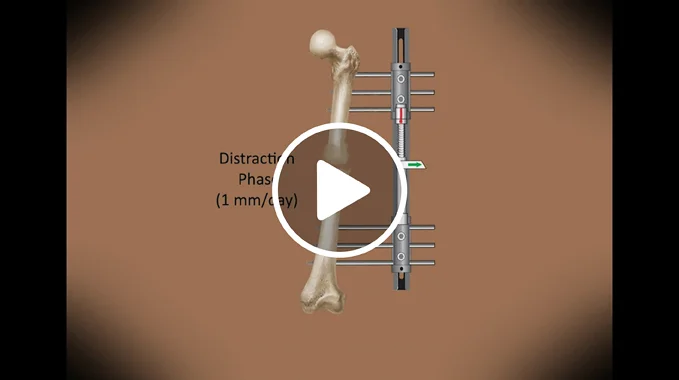
After surgery, the bones are allowed to rest for 5 to 7 days to begin the healing process. After this period of time, the distraction phase of treatment begins. The patient (or family member) will be given a schedule that instructs them how to adjust the fixator several times a day by turning small knobs or other parts of the device to slowly pull the bone segments apart. This gradual process of slowly separating the bone segments is called distraction, which means “pulling apart.” As the bone segments are pulled apart at a slow rate of approximately 1 mm (0.04 inches) per day, new bone forms in the space between them. The new bone is called regenerate bone. The distraction phase lasts until the bone is straight or corrected. The patient will need to see the doctor every 10 to 14 days during the distraction phase.
 After the correction has been achieved, the consolidation phase begins in which the regenerate bone slowly hardens. During this phase of treatment, the external fixator normally remains in place so that it can support the bone as it heals. The bone has consolidated (“healed”) when the regenerate bone has completely hardened and calcified. The consolidation phase typical takes twice as long as the distraction phase. For example, if distraction is completed in 1 month, then consolidation will take 2 months. In this example, the external fixator would remain on the patient for a total of 3 months through both the distraction and consolidation phases.
After the correction has been achieved, the consolidation phase begins in which the regenerate bone slowly hardens. During this phase of treatment, the external fixator normally remains in place so that it can support the bone as it heals. The bone has consolidated (“healed”) when the regenerate bone has completely hardened and calcified. The consolidation phase typical takes twice as long as the distraction phase. For example, if distraction is completed in 1 month, then consolidation will take 2 months. In this example, the external fixator would remain on the patient for a total of 3 months through both the distraction and consolidation phases.
To help the bone heal, patients should avoid nicotine in any form, make sure that their diet includes lots of protein and take vitamin and mineral supplements. During the consolidation phase, your doctor may tell you to start putting some weight on the arm/leg, which will also encourage the bone to harden and heal.
After the bone is fully consolidated, the external fixator can be removed during an outpatient surgical procedure (the patient does not stay in the hospital overnight after the removal procedure). To provide additional protection for the new bone, our doctors may apply a cast or ask the patient to use a brace for 3 to 4 weeks after the external fixator is removed. For more information, please see Limb Lengthening: The Process or Deformity Correction: The Process.
What types of external fixators do the doctors at the International Center for Limb Lengthening use?
 External fixators have many different designs. The two main types are circular/ring external fixators and monolateral external fixators. Both types of external fixators can be hinged to allow the elbow, hip, knee or ankle joint to move during treatment.
External fixators have many different designs. The two main types are circular/ring external fixators and monolateral external fixators. Both types of external fixators can be hinged to allow the elbow, hip, knee or ankle joint to move during treatment.
Circular External Fixators
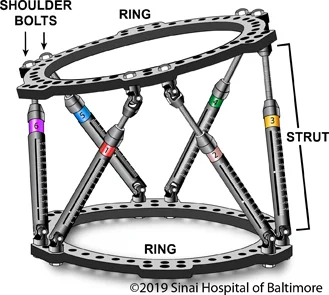
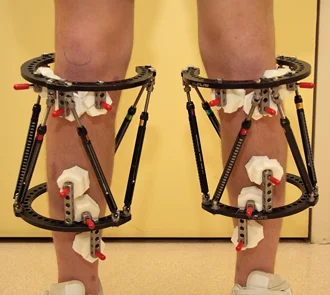
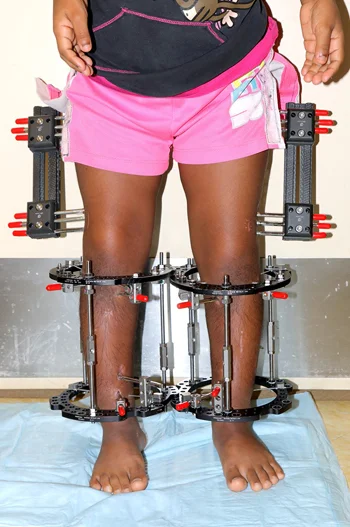
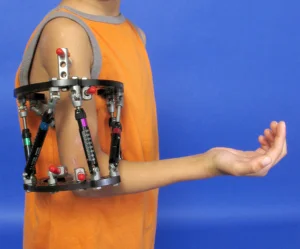
Circular external fixators can completely or partially encircle the arm, leg or foot that is being treated. These fixators are made up of two or more circular rings that are connected by struts, wires or pins.
 The Taylor Spatial Frame (TSF) is one type of circular fixation that we use often. We have published a book on this device entitled The Art of Limb Alignment: Taylor Spatial Frame (Editor: Dr. John E. Herzenberg). The TSF consists of two rings that are connected by six struts. The TSF simultaneously corrects angular, translational and rotational deformities. After the TSF is applied, details about the frame/struts and its position on the body are entered into a computer program. The computer program then generates a correction schedule that instructs the patient (or family member) on how to adjust the TSF several times a day to slowly pull the bone segments apart.
The Taylor Spatial Frame (TSF) is one type of circular fixation that we use often. We have published a book on this device entitled The Art of Limb Alignment: Taylor Spatial Frame (Editor: Dr. John E. Herzenberg). The TSF consists of two rings that are connected by six struts. The TSF simultaneously corrects angular, translational and rotational deformities. After the TSF is applied, details about the frame/struts and its position on the body are entered into a computer program. The computer program then generates a correction schedule that instructs the patient (or family member) on how to adjust the TSF several times a day to slowly pull the bone segments apart.
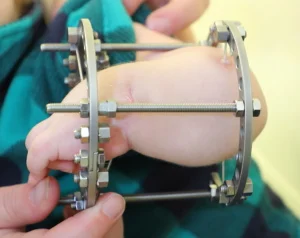 Ilizarov external fixators are another type of circular fixation that we use. The patient (or family member) may need to use a small wrench to adjust the device several times a day. The Ilizarov external fixator was the “original” circular (ring) fixator. It’s use has largely been supplanted by the TSF, but we still occasionally use the classic Ilizarov, particularly in small children.
Ilizarov external fixators are another type of circular fixation that we use. The patient (or family member) may need to use a small wrench to adjust the device several times a day. The Ilizarov external fixator was the “original” circular (ring) fixator. It’s use has largely been supplanted by the TSF, but we still occasionally use the classic Ilizarov, particularly in small children.
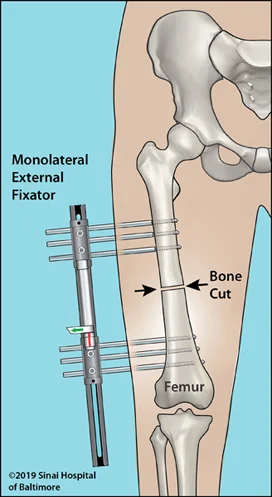
Monolateral External Fixators
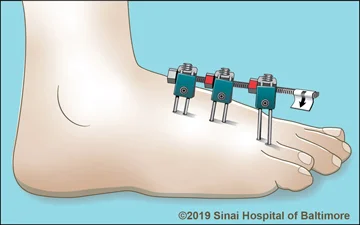
 Monolateral external fixators have a straight bar that is placed on one side of the arm, leg or foot. It is connected to the bone by screws that are often coated with hydroxyapatite to improve the screws’ “hold” in the bone and prevent loosening. The patient (or family member) may need to adjust the device several times a day by turning knobs.
Monolateral external fixators have a straight bar that is placed on one side of the arm, leg or foot. It is connected to the bone by screws that are often coated with hydroxyapatite to improve the screws’ “hold” in the bone and prevent loosening. The patient (or family member) may need to adjust the device several times a day by turning knobs.
What are pin-site infections?
Pin-site infections are the most common problem associated with external fixation treatment. Pin-site infections begin at the level of the skin. If identified early, they are easily treated. If left untreated, they may progress to the deeper soft tissues and possibly even to the bone.
It is important for the patient or family to know the symptoms of a pin-site infection. The most common symptoms are tenderness in an area around a pin site that was not previously tender and increased redness at the pin site. Sometimes the area will have increased warmth, swelling, pain or drainage compared to the other pin sites. Our staff will teach the patient or family more details about these symptoms and proper pin-site care before the patient leaves the hospital.
When patients with external fixation leave the hospital, the doctor will give them a prescription for oral antibiotics. If patients develop the signs of a pin-site infection, they should fill the prescription and immediately begin to take the oral antibiotics. It is important to start the antibiotics quickly (within 24 hours). The patient/family does not need to call the office to confirm that the patient has a pin-site infection before the patient starts taking the oral antibiotics. Once the antibiotics are started, call us within 24 hours to let us know that you are treating a pin-site infection. The redness, tenderness and drainage should improve within 24 to 48 hours of starting the antibiotics.
The risk of a more serious infection (i.e., toxic shock syndrome or necrotizing fasciitis) that can be life-threatening is extremely rare; in over thirty years of applying thousands of external fixators, we have seen fewer than ten patients who have developed such severe infections. The signs of a more serious infection are pin-site pain along with one or more of the following symptoms:
- fever
- fatigue
- rashes
- nausea
- vomiting, and/or
- appearing glassy-eyed, pale or flushed.
If the patient has any of these symptoms, we need to know urgently; contact your doctor or the doctor on call. Again, these types of infection are rare; however, if they occur, treatment is straightforward but must be started immediately. The treatment normally requires a trip to an emergency room and a dose of IV antibiotics for 24 hours.